Empowering Heart Health Through Knowledge
Coronary Calcium Score: Barnacles on a Boat?
In preventative cardiology, one of the most important goals is to identify those who at are risk of developing heart disease, or those who have signs of heart disease so that we can intervene as early as possible to lower the risk of progression of heart disease and having a cardiac event. By cardiac event we mean major adverse cardiac events including heart attack, cardiac arrest or sudden cardiac death, congestive heart failure or stroke as well as other cardiac events including a blockage requiring a stent in the heart or bypass surgery in an elective or semi-elective fashion.
Typically, when approaching preventative cardiac care, all of the traditional cardiac risk factors are evaluated: family history of heart disease, tobacco use history, elevated blood pressure (hypertension), elevated cholesterol, diabetes, prediabetes, metabolic syndrome, obesity. Furthermore, more recently nontraditional cardiac risk factors are also evaluated: chronic inflammatory conditions such as autoimmune disease, poor dental hygiene, obstructive sleep apnea, chronic kidney disease, elevated lipoprotein(a) (also called Lp(a)), elevated uric acid level, air pollution, dietary choices, deconditioning and lack of physical activity, guy microbiota, and vitamin D deficiency.
After identifying which risk factors are present, it is determined if the risk factor can be modified and if the means by which it is altered or modified translates into a lower long term cardiac risk. For example, if someone with elevated blood pressure lowers their blood pressure, to a normal range consistently and long term, their risk of a cardiac event will be reduced going forward.
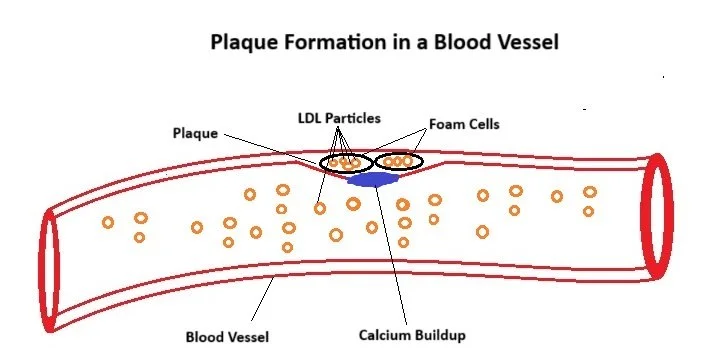
Beyond identifying and modifying risk factors, identifying presence of early cardiac disease can be helpful to reinforce the importance of vigilance in these efforts to lower risk and help with decision making. There are a number of tools to detect the presence of early (or advanced) stages of cardiac disease, for the purposes of this article we will specifically focus on atherosclerotic cardiovascular disease (or plaque build up in the arteries). Some of these tests include a stress test, angiogram, ultrasound of the carotid arteries or arteries in the legs, coronary CT angiogram as well as a coronary calcium score.
What is a coronary calcium score?
A coronary calcium score is a CAT scan (a high resolution X-ray) of the heart which measures the amount of calcium buildup on the coronary arteries, the blood vessels that bring blood flow to the heart itself to keep it supplied with oxygen and nutrients. The score ranges from 0 and can go up to 1000’s if there is extensive calcium buildup. It is important to note that not all plaque buildup in our arteries has calcium on it, so the calcium score doesn’t accurately measure the amount of plaque, but only the plaque that has calcium on it. Early stages of plaque formation typically do not have calcium buildup, but as the plaque progresses, or matures, calcium is often built up on these areas of plaque.
Why is a calcium score helpful?
The coronary calcium score is helpful to determine what our risk over the next decade is for having a cardiac event (heart attack, cardiac arrest, plaque buildup requiring a stent or bypass, or death related to heart disease - in this case the cardiac events are slightly different than above). Additionally, an individual can compare themselves to other individuals in their age and gender category in regards to what percentile they are in, or what percent of individuals in that group have a higher calcium score. Also, a vascular age can be calculated using the calcium score in conjunction with other data to compare to someone’s biologic age.
In practice the calcium score can help gauge an individual’s cardiac risk beyond what traditional risk factors can, as well as help in decision making to choose the right therapy or intervention for lowering cholesterol and aggressiveness of modifying other risk factors.
Atrial Fibrillation: What’s all the fuss?
Atrial fibrillation has become a hot topic in the world of heart health over the past 10-20 years with exciting new advancements in treatment. We set out to discuss what atrial fibrillation is, why it’s important to discuss any potential atrial fibrillation with your doctor, the risk of stroke and heart failure associated with atrial fibrillation, as well as why some individuals are more prone to develop atrial fibrillation and what to do about it.
What is atrial fibrillation?
Atrial fibrillation is an irregular heart rhythm (arrhythmia) that involves the upper chambers of the heart. In normal rhythm, the heart beats sequentially, the two top chambers squeeze the blood to the bottom chambers, and then the bottom chambers pump the blood through both the lungs and the entire body. When atrial fibrillation occurs, the top chambers have unorganized rapid electrical activity that causes them to create a quivering like activity we call fibrillation. This in turn makes the bottom chambers beat irregularly and often very rapid. The presence of atrial fibrillation can cause a variety of symptoms including the sensation of heart racing or beating irregularly (call palpitations), shortness of breath, chest pain, lightheadedness and fatigue to name a few. Additionally, atrial fibrillation increases the risk of stroke by five times compared to those without atrial fibrillation. Atrial fibrillation is more likely to occur in those with high blood pressure, diabetes, sleep apnea, heavy alcohol or caffeine use, as well as those that are overweight.
What are the treatment options for atrial fibrillation?
The most important objective for treatment of atrial fibrillation is determining if a blood thinner is appropriate to reduce the risk of stroke. A healthcare provider will assess an individual’s stroke risk and determine if a blood thinner is appropriate.
Atrial fibrillation is considered a chronic condition, in the sense individuals are rarely “cured” from atrial fibrillation. Although atrial fibrillation may come and go, we can never be sure it will never return. Most treatment discussions center around suppression of atrial fibrillation or reducing the burden of episodes or symptoms related to atrial fibrillation. Atrial fibrillation is generally categorized into two groups, those that are in atrial fibrillation for hours or days at a time (paroxysmal atrial fibrillation) and those that are constantly in atrial fibrillation (persistent atrial fibrillation).
For those individuals with paroxysmal atrial fibrillation, we typically consider two different options, medications call antiarrhythmics, which suppress atrial fibrillation with a 40-50% success rate as well as an ablation procedure which is successful in suppressing atrial fibrillation in 65-70% of individuals at the one-year mark. For individuals that are in atrial fibrillation all the time (persistent atrial fibrillation), we often consider medications called antiarrhythmics that are started prior to a cardioversion, a procedure in which an electrical shock is applied to the chest to stop atrial fibrillation and allow the normal heart rhythm to return. The ablation procedure is also an option for individuals with persistent atrial fibrillation, with a success rate of 50-60%.
An ablation procedure is mostly commonly performed in a hospital setting, in a cardiac catheterization lab. This is a procedure room with highly specialized equipment including a real time x-ray machine, a sophisticated computer system to generate a 3D model of the heart and the equipment to deliver a special type of energy for the ablation itself. During an ablation procedure, a long catheter (similar to a long semi-rigid coated wire) is advanced into the heart to the areas of the heart that are likely responsible for starting atrial fibrillation. Energy is delivered to these areas to render them electrically inactive, or multiple points around other areas to encircle and contain the abnormal electrical signals so they cannot move into the rest of the heart to start atrial fibrillation. The energy delivered can be delivered in two different forms, radiofrequency energy that heats the heart tissue or cryoablation in which the heart tissue is temporarily frozen. Usually, atrial fibrillation is started by a rapid electrical activity in the pulmonary veins (those veins that bring oxygen rich blood back to the left top chamber of the heart). By containing or “isolating” those signals from the rest of the heart, we can suppress atrial fibrillation. Similar to removing a starter on a car engine, it can no longer start up.
What other some other new advances in the area of atrial fibrillation?
An exciting more recent advancement is the use of a device that potentially allows an individual with atrial fibrillation to stop their anticoagulant (a type of blood thinner). These devices are only indicated for use when an individual cannot take a blood thinner long term because of prior major bleeding, such as a bleed inside of the head or in the gastrointestinal tract. The device is placed in an area of the left top chamber of the heart which then blocks blood from entering a small dead end, the left atrial appendage, where most clots for that cause stroke in atrial fibrillation.
Another new advancement in treatment of atrial fibrillation includes a new type of energy for ablation procedures, called pulse field ablation, that can help limit collateral damage to structures near the heart during the ablation procedure.
What can we do other than medications and procedures to help with atrial fibrillation?
A number of measures can be used to help lower the chance of atrial fibrillation returning. These include obtaining quality sleep, treating sleep apnea, reducing or eliminating alcohol use, reducing caffeine intake, weight loss, controlling high blood pressure and optimizing treatment and control of diabetes and blood sugar. In general, sugar free, low processed carbohydrate diets such as Mediterranean diet or DASH diet are recommended. Less common but equality important issues to address include thyroid disorders, inflammatory issues and dehydration and electrolyte abnormalities.
Important Disclaimer:
All questions and concerns regarding atrial fibrillation and heart conditions and treatment should be discussed with a licensed provider. The information found here is educational only and is not meant as a consultation or a substitute for a consultation with your doctor.
The Other “Bad” Cholesterol: Lp(a)
When we look at our cholesterol profile, we usually focus our attention on the “bad” cholesterol particle, the LDL. About 20-30% of individuals have elevated levels of another cholesterol particle, the Lipoprotein(a) also called Lp(a) - a relative of the LDL particle – which puts those individuals at increased risk of having heart disease including plaque formation, heart attack and aortic valve stenosis. Elevated elevates of Lp(a) may increase risk of heart disease by 2 to 3 times compared to those with normal levels. An elevated level of Lp(a) is genetic, meaning it is inherited from one or both of your parents and the level is not significantly influenced by diet.
Who should check their Lp(a) level?
Everyone should have an Lp(a) checked at least once in their life, at the time of a cardiac evaluation or evaluation of cholesterol profile, especially individuals with a strong family history of heart disease including heart attack or plaque build up in their arteries. Additionally, if a first degree relative has an elevated Lp(a) level, you should have your level checked as well. If your Lp(a) level is normal it is unlikely that it needs to be checked again, as a normal Lp(a) level suggests that you have not inherited the genes that cause an elevated level. If it is elevated, it is unclear if it should be checked regularly.
The American Heart Association recommends testing Lp(a) in individuals with borderline or intermediate risk of heart disease as well as those with a family history of premature coronary artery disease.
Why is the Lp(a) associated with a higher risk of heart disease?
The Lp(a) particle is essentially an LDL particle with an additional protein attached to it called apolipoprotein(a), and that additional protein increases the risk of heart attack through a number of ways. Lp(a) can increase the risk of forming a clot, promote inflammation and formation of plaque in the arteries.
What can I do about an elevated Lp(a)?
The presence of an elevated Lp(a) value (greater than 125 nmol/L or 50 mg/dL) increases the risk of heart disease including heart attack. It is unclear if taking medications that lower Lp(a) will lower your risk of heart disease. Medications such as niacin and PCSK9 inhibitors(such as evolocumab aka Repatha) do lower Lp(a) but a reduction in risk of heart attack has not been demonstrated in those patients specifically. Apheresis is a procedure that can filter Lp(a) from your blood, reducing levels up to 50%, but is a significant burden as it required regular treatments. There are a number of medications in clinical trials specifically targeting lowering Lp(a), which will potentially provide a therapy for reducing heart disease risk in patients with high Lp(a) levels.
In the meantime, aggressively lowering modifiable risk factors remains the focus of cardiac disease risk reduction in patients with Lp(a) including aggressively lowering LDL, managing blood sugar, avoidance of tobacco, optimizing diet (such as Mediterranean diet), regular dental cleanings and treating any inflammatory conditions.
There may be a role for aspirin for reducing the risk of heart attack in those with Lp(a), but the decision to start aspirin should be discussed with a licensed provider.
All questions and concerns regarding Lp(a) and treatment should be discussed with a licensed provider. The information found here is educational only and is not meant as a consultation or a substitute for a consultation with your doctor.
What is Cholesterol and Why Does it Cause Heart Disease?
It all begins with an idea.
The story of cholesterol begins with understanding what cholesterol is, why it is important for us and why it can also be harmful.
Cholesterol is a complex molecule that is both absorbed into the body by our gut from the food we eat, and manufactured in the liver and brain from basic building blocks. It is essential for life and found in all cells of the body – and a basic building block for parts of cell membranes, production of hormones and other important molecules in the body.
The problem with cholesterol is when it is present in abundance in cholesterol carrying particles called LDL. The LDL particles have an outer shell or membrane with the inside containing cholesterol and other molecules including triglycerides, as well as a protein attached to the outside (apolipoprotein B) to tag it as an LDL particle, similar to a bar code or name tag. These LDL particles shuttle cholesterol through the blood stream from the liver to parts of the body that need cholesterol for healthy function. When these LDL particles find their way into the lining of blood vessels, plaque may form, which leads to heart disease and other forms of cardiovascular disease.
Why do LDL cholesterol particles form plaque in some people but not others?
Cholesterol carrying LDL particles find their way into the lining of blood vessels and start the formation of plaque for a variety of reasons. To begin with, think of the lining of blood vessels as a tight knit patch work sealing the contents of blood from leaving the blood vessel. Certain factors making that lining more permeable less “watertight,” allowing the LDL cholesterol particles to slip into the layers of the blood vessel. When those LDL particles are in the lining of the blood vessel, they are susceptible to a process called oxidation which chemically alters them. Oxidation is a chemical process that is more likely when inflammation is present in the body. When the house keeping cells of the body called macrophages find these LDL particles, they “eat” the LDL particles and form foam cells which is the early stages of plaque and atherosclerotic cardiovascular disease (ASCVD).
What can we do to reduce the risk of heart attack and cardiovascular disease?
By reducing the factors that lead to plaque, we can reduce the chance of plaque formation and heart attack. There are two main ways to achieve this, reduce the amount of LDL particles or make the lining of our blood vessels healthier or “watertight” so that the LDL particles cannot escape to the outer lining to start the plaque formation process.
How to reduce cholesterol LDL particles?
There are a number of ways to lower the LDL particle number in our blood, both through diet and medication. Generally, a sugar free, low processed carbohydrate diet such as Mediterranean diet or DASH diet are recommended to help with cholesterol. High fiber diets may reduce the absorption of cholesterol. A variety of medications are available to reduce cholesterol, including statins, ezetimibe (which reduces absorption or cholesterol from the gut), PCSK9 inhibitors that allow the liver to eliminate more LDL particles from the blood in addition to a number of other agents.
How can I make the lining of my blood vessels healthier to lower my heart disease risk?
We look at “risk factors” for heart disease and by addressing them we can improve the health of our blood vessels. Controlling blood pressure, treating diabetes through diet and weight loss as well as medication, avoiding tobacco products, lowering cholesterol LDL particles in the blood, regular dental cleanings and reducing the amount of inflammation in the body.